Abstract
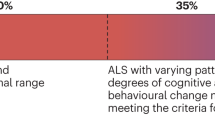
Increasing appreciation of the phenotypic and biological overlap between amyotrophic lateral sclerosis (ALS) and frontotemporal dementia, alongside evolving biomarker evidence for a pre-symptomatic stage of disease and observations that this stage of disease might not always be clinically silent, is challenging traditional views of these disorders. These advances have highlighted the need to adapt ingrained notions of these clinical syndromes to include both the full phenotypic continuum — from clinically silent, to prodromal, to clinically manifest — and the expanded phenotypic spectrum that includes ALS, frontotemporal dementia and some movement disorders. The updated clinical paradigms should also align with our understanding of the biology of these disorders, reflected in measurable biomarkers. The Miami Framework, emerging from discussions at the Second International Pre-Symptomatic ALS Workshop in Miami (February 2023; a full list of attendees and their affiliations appears in the Supplementary Information) proposes a classification system built on: first, three parallel phenotypic axes — motor neuron, frontotemporal and extrapyramidal — rather than the unitary approach of combining all phenotypic elements into a single clinical entity; and second, biomarkers that reflect different aspects of the underlying pathology and biology of neurodegeneration. This framework decouples clinical syndromes from biomarker evidence of disease and builds on experiences from other neurodegenerative diseases to offer a unified approach to specifying the pleiotropic clinical manifestations of disease and describing the trajectory of emergent biomarkers.
Key points
-
Amyotrophic lateral sclerosis, frontotemporal dementia and a group of extrapyramidal movement disorders are related across a phenotypic spectrum and have shared biological substrates such as TDP43 or tau pathology.
-
Disease evolves along a phenotypic continuum from clinically silent, to prodromal, to clinically manifest disease. Existing diagnostic criteria might require updates given new knowledge of prodromal and early manifest disease.
-
Biomarkers reflecting the underlying biology of these diseases and the resulting neurodegenerative changes have begun to emerge, but the temporal relationship of the biomarkers to clinical phenotypes is unclear.
-
The Miami Framework offers a unified approach to specifying both the pleotropic clinical manifestations of these diseases and, in parallel, the temporal course of emergent biomarkers.
-
Informed by data and experience from multiple genetic forms of amyotrophic lateral sclerosis and frontotemporal dementia, the Miami Framework probably has relevance to all forms of these diseases.
-
Communicating the emergence of prodromal disease to the affected individual is complex and requires great caution but can be informed by experience and insights from genetic and biomarker counselling.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
29 May 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41582-024-00978-4
References
Clinical and neuropathological criteria for frontotemporal dementia. The Lund and Manchester Groups. J. Neurol. Neurosurg. Psychiatry 57, 416–418 (1994).
Brooks, B. R., Miller, R. G., Swash, M. & Munsat, T. L. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. Other Mot. Neuron Disord. 1, 293–299 (2000).
de Carvalho, M. et al. The Awaji criteria for diagnosis of ALS. Muscle Nerve 44, 456–457 (2011).
Ludolph, A. et al. A revision of the El Escorial criteria — 2015. Amyotroph. Lateral Scler. Frontotemporal Degener. 16, 291–292 (2015).
Neary, D. & Snowden, J. Frontal lobe dementia, motor neuron disease, and clinical and neuropathological criteria. J. Neurol. Neurosurg. Psychiatry 84, 713–714 (2013).
Neary, D. et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology 51, 1546–1554 (1998).
Rascovsky, K. et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 134, 2456–2477 (2011).
Shefner, J. M. et al. A proposal for new diagnostic criteria for ALS. Clin. Neurophysiol. 131, 1975–1978 (2020).
Strong, M. J. et al. Amyotrophic lateral sclerosis — frontotemporal spectrum disorder (ALS-FTSD): Revised diagnostic criteria. Amyotroph. Lateral Scler. Frontotemporal Degener. 18, 153–174 (2017).
Benatar, M. et al. Mild motor impairment as prodromal state in amyotrophic lateral sclerosis: a new diagnostic entity. Brain 145, 3500–3508 (2022).
Benatar, M., Wuu, J., Andersen, P. M., Lombardi, V. & Malaspina, A. Neurofilament light: a candidate biomarker of pre-symptomatic ALS and phenoconversion. Ann. Neurol. 84, 130–139 (2018).
Bjornevik, K. et al. Prediagnostic neurofilament light chain levels in amyotrophic lateral sclerosis. Neurology 97, e1466–e1474 (2021).
Smith, E. N. et al. Plasma neurofilament light levels show elevation two years prior to diagnosis of amyotrophic lateral sclerosis in the UK Biobank. Amyotroph. Lateral Scler. Frontotemporal Degener. 25, 170–176 (2024).
Benatar, M. et al. Preventing amyotrophic lateral sclerosis: insights from pre-symptomatic neurodegenerative diseases. Brain 145, 27–44 (2022).
Boeve, B. F., Boxer, A. L., Kumfor, F., Pijnenburg, Y. & Rohrer, J. D. Advances and controversies in frontotemporal dementia: diagnosis, biomarkers, and therapeutic considerations. Lancet Neurol. 21, 258–272 (2022).
Benussi, A. et al. Conceptual framework for the definition of preclinical and prodromal frontotemporal dementia. Alzheimers Dement. 18, 1408–1423 (2022).
Mitsumoto, H., Kasarskis, E. J. & Simmons, Z. Hastening the diagnosis of amyotrophic lateral sclerosis. Neurology 99, 60–68 (2022).
Benatar, M. & Wuu, J. Presymptomatic studies in ALS: rationale, challenges, and approach. Neurology 79, 1732–1739 (2012).
Estevez-Fraga, C. et al. Expanding the spectrum of movement disorders associated with C9orf72 hexanucleotide expansions. Neurol. Genet. 7, e575 (2021).
Daube, J. R. Electrodiagnostic studies in amyotrophic lateral sclerosis and other motor neuron disorders. Muscle Nerve 23, 1488–1502 (2000).
Swash, M. Shortening the time to diagnosis in ALS: the role of electrodiagnostic studies. Amyotroph. Lateral Scler. Other Mot. Neuron Disord. 1, S67–S72 (2000).
Johnsen, B. et al. Diagnostic criteria for amyotrophic lateral sclerosis: a multicentre study of inter-rater variation and sensitivity. Clin. Neurophysiol. 130, 307–314 (2019).
Petersen, R. C. Mild cognitive impairment as a diagnostic entity. J. Intern. Med. 256, 183–194 (2004).
Benatar, M., Turner, M. R. & Wuu, J. Defining pre-symptomatic amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. Frontotemporal Degener. 20, 303–309 (2019).
Brooks, B. R. The role of axonal transport in neurodegenerative disease spread: a meta-analysis of experimental and clinical poliomyelitis compares with amyotrophic lateral sclerosis. Can. J. Neurological Sci. 18, 435–438 (1991).
Grossman, M. et al. Frontotemporal lobar degeneration. Nat. Rev. Dis. Prim. 9, 40 (2023).
Leroy, M. et al. Characteristics and progression of patients with frontotemporal dementia in a regional memory clinic network. Alzheimers Res. Ther. 13, 19 (2021).
Boeve, B. et al. The longitudinal evaluation of familial frontotemporal dementia subjects protocol: Framework and methodology. Alzheimers Dement. 16, 22–36 (2020).
Olney, N. T. et al. Clinical and volumetric changes with increasing functional impairment in familial frontotemporal lobar degeneration. Alzheimers Dement. 16, 49–59 (2020).
Barker, M. S. et al. Proposed research criteria for prodromal behavioural variant frontotemporal dementia. Brain 145, 1079–1097 (2022).
Brooks, B. R. El Escorial World Federation of Neurology Criteria for the diagnosis of amyotrophic lateral sclerosis. J. Neurological Sci. 124, 96–107 (1994).
Taylor, L. J. et al. Is language impairment more common than executive dysfunction in amyotrophic lateral sclerosis? J. Neurol. Neurosurg. Psychiatry 84, 494–498 (2013).
Abrahams, S. Executive dysfunction in ALS is not the whole story. J. Neurol. Neurosurg. Psychiatry 84, 474–475 (2013).
Saxon, J. A. et al. Semantic dementia, progressive non-fluent aphasia and their association with amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry 88, 711–712 (2017).
Kendler, K. S. The phenomenology of major depression and the representativeness and nature of DSM criteria. Am. J. Psychiatry 173, 771–780 (2016).
Tipton, P. W. et al. Differences in motor features of C9orf72, MAPT, or GRN variant carriers with familial frontotemporal lobar degeneration. Neurology 99, e1154–e1167 (2022).
Siuda, J., Fujioka, S. & Wszolek, Z. K. Parkinsonian syndrome in familial frontotemporal dementia. Parkinsonism Relat. Disord. 20, 957–964 (2014).
Rowe, J. B., Holland, N. & Rittman, T. Progressive supranuclear palsy: diagnosis and management. Pract. Neurol. 21, 376–383 (2021).
Espay, A. J. & Litvan, I. Parkinsonism and frontotemporal dementia: the clinical overlap. J. Mol. Neurosci. 45, 343–349 (2011).
de Pablo-Fernandez, E. et al. A clinicopathologic study of movement disorders in frontotemporal lobar degeneration. Mov. Disord. 36, 632–641 (2021).
Gasca-Salas, C. et al. Characterization of movement disorder phenomenology in genetically proven, familial frontotemporal lobar degeneration: a systematic review and meta-analysis. PLoS ONE 11, e0153852 (2016).
Baizabal-Carvallo, J. F. & Jankovic, J. Parkinsonism, movement disorders and genetics in frontotemporal dementia. Nat. Rev. Neurol. 12, 175–185 (2016).
Wen, Y., Zhou, Y., Jiao, B. & Shen, L. Genetics of progressive supranuclear palsy: a review. J. Parkinsons Dis. 11, 93–105 (2021).
Foster, N. L. et al. Frontotemporal dementia and parkinsonism linked to chromosome 17: a consensus conference. Conference Participants. Ann. Neurol. 41, 706–715 (1997).
Fiondella, L. et al. Movement disorders are linked to TDP-43 burden in the substantia nigra of FTLD-TDP brain donors. Acta Neuropathol. Commun. 11, 63 (2023).
Arienti, F. et al. Unravelling genetic factors underlying corticobasal syndrome: a systematic review. Cells 10, 171 (2021).
Steele, J. C. Parkinsonism-dementia complex of Guam. Mov. Disord. 20, S99–S107 (2005).
Hensman Moss, D. J. et al. C9orf72 expansions are the most common genetic cause of Huntington disease phenocopies. Neurology 82, 292–299 (2014).
Armstrong, M. J. et al. Criteria for the diagnosis of corticobasal degeneration. Neurology 80, 496–503 (2013).
Hoglinger, G. U. et al. Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria. Mov. Disord. 32, 853–864 (2017).
Benatar, M., Turner, M. R. & Wuu, J. Presymptomatic amyotrophic lateral sclerosis: from characterization to prevention. Curr. Opin. Neurol. 36, 360–364 (2023).
Gorno-Tempini, M. L. et al. Classification of primary progressive aphasia and its variants. Neurology 76, 1006–1014 (2011).
Jack, C. R. Jr. et al. NIA-AA Research Framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 14, 535–562 (2018).
Jack, C. R. Jr. et al. A/T/N: An unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology 87, 539–547 (2016).
Hoglinger, G. U. et al. A biological classification of Parkinson’s disease: the SynNeurGe research diagnostic criteria. Lancet Neurol. 23, 191–204 (2024).
Benatar, M. et al. Neurofilaments in pre-symptomatic ALS and the impact of genotype. Amyotroph. Lateral Scler. Frontotemporal Degener. 20, 538–548 (2019).
Meeter, L. H. et al. Neurofilament light chain: a biomarker for genetic frontotemporal dementia. Ann. Clin. Transl. Neurol. 3, 623–636 (2016).
van der Ende, E. L. et al. Serum neurofilament light chain in genetic frontotemporal dementia: a longitudinal, multicentre cohort study. Lancet Neurol. 18, 1103–1111 (2019).
Rojas, J. C. et al. Plasma neurofilament light for prediction of disease progression in familial frontotemporal lobar degeneration. Neurology 96, e2296–e2312 (2021).
Saracino, D. et al. Plasma NfL levels and longitudinal change rates in C9orf72 and GRN-associated diseases: from tailored references to clinical applications. J. Neurol. Neurosurg. Psychiatry 92, 1278–1288 (2021).
Gendron, T. F. et al. Comprehensive cross-sectional and longitudinal analyses of plasma neurofilament light across FTD spectrum disorders. Cell Rep. Med. 3, 100607 (2022).
Wilke, C. et al. Stratifying the presymptomatic phase of genetic frontotemporal dementia by serum NfL and pNfH: a longitudinal multicentre study. Ann. Neurol. 91, 33–47 (2022).
Staffaroni, A. M. et al. Temporal order of clinical and biomarker changes in familial frontotemporal dementia. Nat. Med. 28, 2194–2206 (2022).
Benatar, M., Wuu, J. & Turner, M. R. Neurofilament light chain in drug development for amyotrophic lateral sclerosis: a critical appraisal. Brain 146, 2711–2716 (2023).
Irwin, D. J. et al. Ante mortem cerebrospinal fluid tau levels correlate with postmortem tau pathology in frontotemporal lobar degeneration. Ann. Neurol. 82, 247–258 (2017).
Cousins, K. A. Q. et al. Elevated plasma phosphorylated Tau 181 in amyotrophic lateral sclerosis. Ann. Neurol. 92, 807–818 (2022).
Saijo, E. et al. 4-Repeat tau seeds and templating subtypes as brain and CSF biomarkers of frontotemporal lobar degeneration. Acta Neuropathologica 139, 63–77 (2020).
Chatterjee, M. et al. Plasma extracellular vesicle Tau isoform ratios and TDP-43 inform about molecular pathology in frontotemporal dementia and amyotrophic lateral sclerosis. Preprint at ResSq. https://doi.org/10.21203/rs.3.rs-3158170/v1 (2023).
Irwin, K. E. et al. A fluid biomarker reveals loss of TDP-43 splicing repression in presymptomatic ALS–FTD. Nat. Med. 30, 382–393 (2024).
Andersen, P. M. et al. EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS)-revised report of an EFNS task force. Eur. J. Neurol. 19, 360–375 (2012).
Pressman, P. S. & Miller, B. L. Diagnosis and management of behavioral variant frontotemporal dementia. Biol. Psychiatry 75, 574–581 (2014).
Arias, J. J. & Karlawish, J. Confidentiality in preclinical Alzheimer disease studies: when research and medical records meet. Neurology 82, 725–729 (2014).
United States. The Genetic Information Nondiscrimination Act of 2008 (GINA). In: US Department of Labor EBSA, editor. Public Law No 110-233 (Washington, DC, 2008).
Prince, A. E. & Berkman, B. E. When does an illness begin: genetic discrimination and disease manifestation. J. Law Med. Ethics 40, 655–664 (2012).
Benatar, M. et al. Design of a randomized, placebo-controlled, phase 3 trial of tofersen initiated in clinically presymptomatic SOD1 variant carriers: the ATLAS study. Neurotherapeutics 19, 1248–1258 (2022).
Largent, E. A. et al. Testing for Alzheimer disease biomarkers and disclosing results across the disease continuum. Neurology 100, 1010–1019 (2023).
Bourinaris, T. & Houlden, H. C9orf72 and its relevance in parkinsonism and movement disorders: a comprehensive review of the literature. Mov. Disord. Clin. Pract. 5, 575–585 (2018).
Benatar, M. et al. Validation of serum neurofilaments as prognostic and potential pharmacodynamic biomarkers for ALS. Neurology 95, e59–e69 (2020).
Feneberg, E. et al. Multicenter evaluation of neurofilaments in early symptom onset amyotrophic lateral sclerosis. Neurology 90, e22–e30 (2018).
Lu, C. H. et al. Neurofilament light chain: a prognostic biomarker in amyotrophic lateral sclerosis. Neurology 84, 2247–2257 (2015).
Poesen, K. et al. Neurofilament markers for ALS correlate with extent of upper and lower motor neuron disease. Neurology 88, 2302–2309 (2017).
Thompson, A. G. et al. Multicentre appraisal of amyotrophic lateral sclerosis biofluid biomarkers shows primacy of blood neurofilament light chain. Brain Commun. 4, fcac029 (2022).
Wilke, C. et al. Serum neurofilament light chain is increased in hereditary spastic paraplegias. Ann. Clin. Transl. Neurol. 5, 876–882 (2018).
Shepheard, S. et al. Urinary p75 extracellular domain; a biomarker for prognosis, progression and pharmacodynamic effect in ALS. Neurology 88, 1137–1143 (2017).
Gertsman, I. et al. An endogenous peptide marker differentiates SOD1 stability and facilitates pharmacodynamic monitoring in SOD1 amyotrophic lateral sclerosis. JCI Insight 4, e122768 (2019).
Turner, M. R. et al. Primary lateral sclerosis: consensus diagnostic criteria. J. Neurol. Neurosurg. Psychiatry 91, 373–377 (2020).
Acknowledgements
We are indebted to participants in the Pre-Symptomatic Familial ALS (Pre-fALS) and ARTFL LEFFTDS Longitudinal FTD (ALLFTD) studies for their contribution to research. Data and insights from these studies provided a foundation for discussions at the Second International Pre-Symptomatic ALS Workshop. The Second International Pre-Symptomatic ALS Workshop was made possible through the generous support of the ALS Association, the Association for Frontotemporal Degeneration, the Muscular Dystrophy Association, the Motor Neurone Disease Association of England, Wales and Northern Ireland, Biogen, Eli Lilly, Novartis, Regeneron, uniQure and the National Institutes of Health (U54-NS092091).
Author information
Authors and Affiliations
Consortia
Contributions
M.B. prepared the initial draft of the manuscript. J.W., M.R.T., A.A.-C., E.D.H., C.T.M., R.C.P., and R.P. substantively edited the initial draft. All authors contributed to discussion of the content, and reviewed or edited the manuscript. M.B. and J.W. prepared the figures and finalized the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
M.B. receives consulting fees for Alector, Alexion, Annexon, Arrowhead, Biogen, Cartesian, Denali, Eli Lilly, Horizon, Immunovant, Novartis, Roche, Sanofi, Takeda, UCB and UniQure. The University of Miami has licensed intellectual property to Biogen to support design of the ATLAS study. R.C.P. reports consulting for Roche, Genentech, Eli Lilly and Co., Eisai, and Nestle. R.P. reports grants and personal fees from Fonds de la Recherche en Sante, grants from the Canadian Institute of Health Research, the Michael J. Fox Foundation, the National Institute of Health, Roche and the Webster Foundation, and personal fees from Takeda, Abbvie, Biogen, Bristol Myers Squibb, Curasen, Eisai, the International Parkinson and Movement Disorders Society, Korro, Lilly, Merck, Novartis, Paladin, Parkinson Canada, and Vaxxinity outside the submitted work. L.D. reports consulting for Biogen, MJH Life Sciences, Passage Bio and Sano Genetics. N.T. is an employee of the ALS Association. A.B. has served as a paid consultant to AGTC, Alector, Alzprotect, Amylyx, Arkuda, Arrowhead, Arvinas, Aviado, Boehringer Ingelheim, Denali, Eli Lilly, GSK, Humana, Life Edit, Merck, Modalis, Oligomerix, Oscotec, Roche, Transposon and Wave. B.F.B. reports honoraria for scientific advisory board activities for the Tau Consortium, funded by the Rainwater Charitable Foundation, and institutional research grant support for clinical trials from Alector, Biogen, Cognition Therapeutics, EIP Pharma, GE Healthcare and Transposon. P.D. is an employee of Association for Frontotemporal Degeneration. P.L. reports honoraria for advisory boards, consultancies or speaker remuneration from Abbvie, Alexion, Bial, Desitin, ITF Pharma, Novartis Pharma, Stada Pharm, Woolsey Pharma and Zambon. He is a co-inventor on patents EP 2825175 B1, US 9.980,972 B2 for the treatment of ALS. His work on ALS is funded by the Bundesministerium für Bildung und Forschung (01ED2204A, 01GM1917A, 01GM1704A/B), the Deutsche Forschungsgemeinschaft (SyNergy project-ID 390857198) and the Deutsche Gesellschaft für Muskelkranke (DGM). P.M.A. reports paid consultancies and serves/has served on advisory boards for Arrowhead, Avrion, Biogen, Orphazyme, Regeneron, Roche, and uniQure and as clinical trial site investigator for AB Science, Alexion Pharmaceuticals, AL-S Pharma and Lilly, Amylyx, Biogen Idec, IONIS Pharmaceuticals, Orion Pharma, Rhône-Poulenc and Sanofi. Since 1993, he has been Director of the ALS-genetic laboratory at Umeå University Hospital, which performs not-for-profit research genetic testing. He is a member of the ClinGen ALS Gene variant Curation Expert panel. A.A.-C. reports consultancies or advisory boards for Amylyx, Apellis, Biogen, Brainstorm, Cytokinetics, GenieUs, GSK, Lilly, Mitsubishi Tanabe Pharma, Novartis, Orion Pharma, Quralis, Sano, Sanofi and Wave Pharmaceuticals, and the following patent: “Use of CSF-Neurofilament determinations and CSF-Neurofilament thresholds of prognostic and stratification value with regards to response to therapy in neuromuscular and neurodegenerative diseases”. The other authors report no conflicts of interest.
Peer review
Peer review information
Nature Reviews Neurology thanks Adriano Chiò, Orla Hardiman and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ALLFTD: https://www.allftd.org/
Spectrum Disorders Gene Curation: https://clinicalgenome.org/affiliation/40096/
Variant Curation Expert Panels: https://clinicalgenome.org/affiliation/50096/
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benatar, M., Wuu, J., Huey, E.D. et al. The Miami Framework for ALS and related neurodegenerative disorders: an integrated view of phenotype and biology. Nat Rev Neurol (2024). https://doi.org/10.1038/s41582-024-00961-z
Accepted:
Published:
DOI: https://doi.org/10.1038/s41582-024-00961-z